Artificial intelligence is rapidly advancing in the medical field, with new programs demonstrating capabilities in diagnosis and data analysis that in some cases surpass those of human physicians. This technological shift is prompting a fundamental re-evaluation of the role of doctors, who are beginning to integrate AI into their practices while navigating its potential to reshape their profession.
From triaging patients to interpreting complex medical scans, AI tools are no longer theoretical concepts but active participants in patient care. This integration is forcing medical professionals to ask a critical question: In an age of intelligent machines, what is the core purpose of a human doctor?
Key Takeaways
- Artificial intelligence is demonstrating advanced diagnostic and data analysis capabilities, sometimes outperforming human doctors.
- Specialists are using AI-powered bots to triage patients, improving access for those with the most urgent needs.
- While AI excels at pattern recognition and administrative tasks, doctors emphasize the irreplaceable value of human intuition, empathy, and interpreting subtle patient cues.
- Experts raise concerns about AI perpetuating existing biases and being used to optimize a flawed healthcare system for profit rather than patient benefit.
- The medical community is adapting, viewing AI as a tool that could handle routine tasks, allowing doctors to focus more on complex cases and the human side of medicine.
The Rise of the Digital Colleague
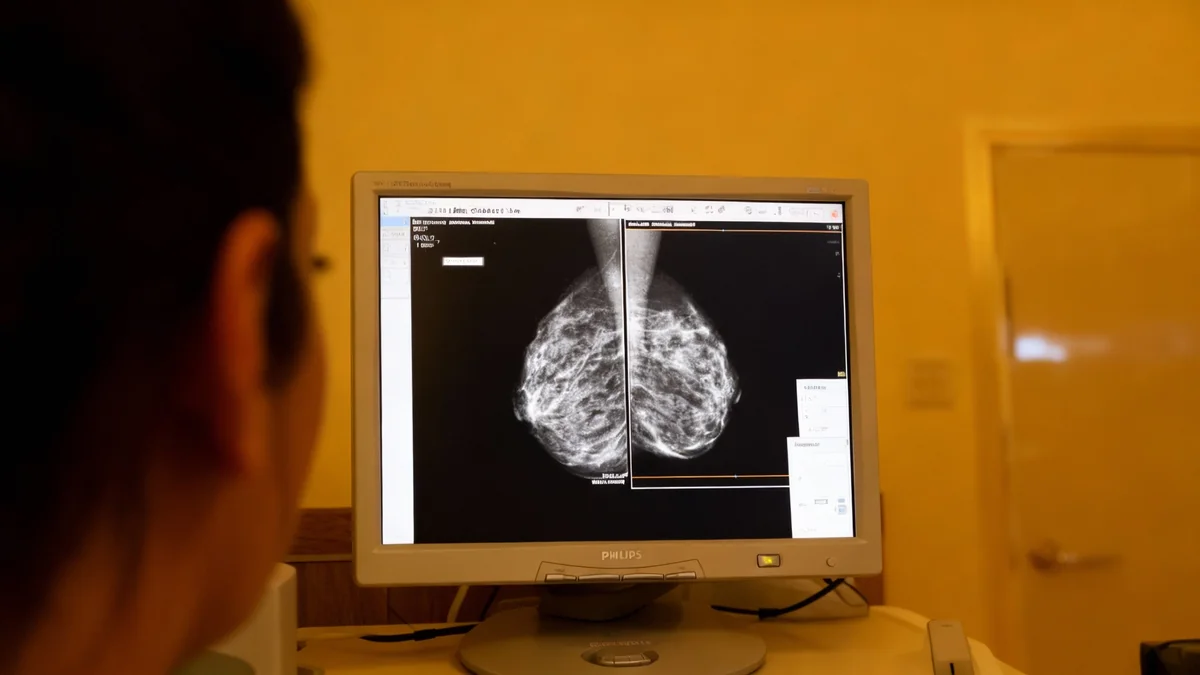
In clinics and hospitals, AI is transitioning from a futuristic idea to a daily tool. Some physicians report that AI's ability to analyze data and formulate diagnoses is already outpacing human capacity in specific areas. The technology is proving adept at reading scans and images with a high degree of accuracy, answering patient questions through online portals, and even drafting appeals to insurance companies.
This has led to what some describe as an existential moment for the medical community. Dr. Jonathan Chen, an internist at Stanford, has even practiced difficult patient conversations with a chatbot to refine his approach. He notes that the proficiency of these programs can be unsettling, forcing physicians to consider which tasks might be better handled by a machine.
Dr. Harlan Krumholz, a cardiologist at Yale, agrees that AI's reasoning abilities are advancing quickly. "A.I.’s reasoning and ability to make diagnoses is already outpacing what physicians can do," he stated, highlighting the rapid pace of change.
Redefining Medical Expertise
Despite AI's power, medical experts caution that it is not yet ready to replace human doctors. The core of medical practice often lies in understanding nuance that data alone cannot capture. Dr. Lee Schwamm, a neurologist at Yale School of Medicine, points out the complexities of human communication.
"The patient says, ‘Yesterday I woke up dizzy. My arm was dead, and I had trouble speaking.’ What does ‘dizzy’ actually mean?" Dr. Schwamm explained. It could imply lightheadedness or a spinning room—two very different symptoms with different implications.
This is where human experience becomes critical. A seasoned physician can interpret subtle cues, synthesize incomplete information, and apply clinical judgment built over years of practice. According to Dr. Schwamm, AI is excellent at matching patterns from the data it's given, but it "has no way to extract that information itself."
AI's Diagnostic Edge
In certain applications, AI has already proven superior to human experts. For instance, AI algorithms can analyze an electrocardiogram (ECG) and detect patterns indicative of heart conditions that are invisible to the human eye of a cardiologist. This allows for earlier and more accurate diagnoses, potentially by general practitioners instead of specialists.
Furthermore, the human connection remains central to patient care, especially when delivering life-altering news. Explaining a serious diagnosis and discussing treatment options requires empathy and a level of understanding that machines currently lack.
A Tool for a Strained System
One of the most immediate applications for AI is in alleviating pressure on an overburdened healthcare system. Long wait times to see specialists are a common problem, and AI is helping to streamline patient flow.
Dr. John Erik Pandolfino, a specialist at Northwestern University's Feinberg School of Medicine, developed an AI solution called GERDBot to manage patients with gastroesophageal reflux disease. The bot triages incoming cases by asking questions, identifying those with severe symptoms who need to be seen immediately.
This system allows patients with less critical conditions to receive prompt attention from a nurse practitioner or physician assistant, while freeing up Dr. Pandolfino to focus on the most complex cases. "Most people are appreciative that they get started with their care and get information right away," he said.
Addressing the Doctor Shortage
The United States faces a significant shortage of primary care physicians, affecting both rural and urban areas. Dr. Isaac Kohane of Harvard Medical School noted the difficulty of finding a primary care doctor in Boston, a city with numerous hospitals. AI is seen as a potential tool to extend the reach of existing doctors by empowering nurse practitioners and other medical staff to handle more routine care, thereby improving patient access.
The goal is to use technology to make healthcare more efficient. By automating administrative duties and assisting with initial diagnoses, AI could allow doctors to see more patients with complex needs, reducing the months-long waits that many currently endure.
Navigating the Risks and Biases
The deployment of AI in healthcare is not without challenges. A primary concern is that these systems could inherit and amplify existing biases present in the medical data they are trained on. Studies have shown that some algorithms might pay less attention to symptoms from women or individuals who make grammatical errors in their written communications.
Dr. Leo Anthony Celi of M.I.T. expressed a broader concern. "The real concern isn’t A.I. itself," he said. "It’s that A.I. is being deployed to optimize a profoundly broken system rather than to reimagine it." There is a risk that healthcare systems will use AI primarily to increase billing efficiency or replace staff, rather than to improve patient outcomes.
However, proponents like Dr. Adam Rodman, an internist at Beth Israel Deaconess Medical Center, argue that these risks should not halt progress. He believes that because AI's biases can be documented and measured, there is an opportunity to correct them—a task that is much harder with inherent human biases.
The Future of the Physician
As AI handles more of the routine, data-driven tasks, the role of the doctor is expected to evolve. Many physicians, like Dr. Jeffrey A. Linder of Northwestern, welcome the idea of offloading the "check the box" aspects of primary care. This would allow them to focus on what drew them to medicine: the human element.
The consensus is that medicine is changing irreversibly. The future physician may act more like a skilled interpreter and guide, using AI as a powerful assistant while retaining final authority and, most importantly, managing the patient relationship.
As Dr. Joshua Steinberg, a primary care physician at SUNY Upstate Medical University, puts it, the core of the profession will remain. "Even if an A.I. has read all the medical literature, I will still be the expert on my patients," he said. "I think our doctoring role may look a little different, but I will still be sitting on a little rolling stool, talking to the patient."