Scientists have successfully used artificial intelligence to identify two new biological subtypes of multiple sclerosis, a significant development that could reshape how the condition is diagnosed and treated. The discovery, based on a combination of blood tests and MRI scans, moves beyond symptom-based classifications to the underlying biology of the disease, opening the door for personalized medical care.
The research, led by University College London (UCL), offers a new framework for understanding the progression of MS, potentially allowing doctors to predict which patients are at a higher risk of complications and tailor treatments more effectively.
Key Takeaways
- Researchers used an AI model to analyze blood tests and MRI scans from 600 patients.
- Two distinct biological subtypes of multiple sclerosis, named 'early sNfL' and 'late sNfL', were discovered.
- The findings could enable doctors to provide personalized treatments based on a patient's specific disease pattern.
- This new classification method focuses on the underlying biological changes rather than clinical symptoms.
A New Era for MS Diagnostics
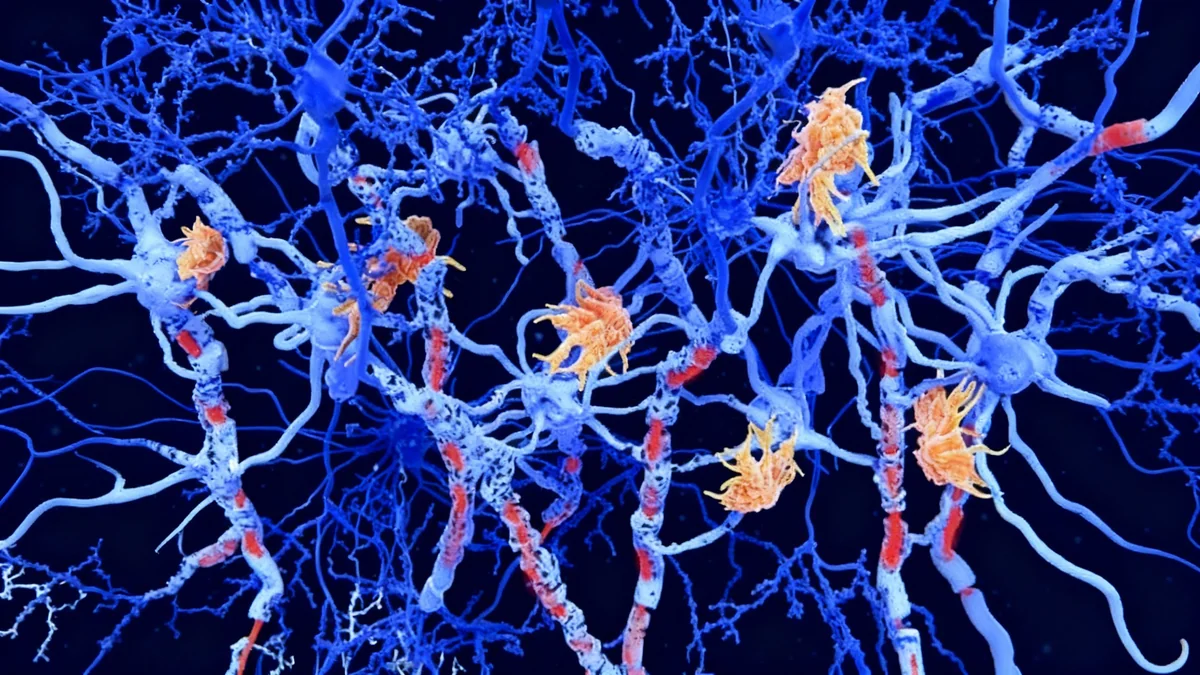
For decades, multiple sclerosis has been categorized based on a patient's observable symptoms, such as whether they experience relapses or steady progression. However, this approach does not always reflect the specific biological processes occurring within an individual's nervous system. Millions of people live with MS globally, and treatment is often a process of trial and error.
A new study published in the journal Brain details how researchers have pioneered a method to see past symptoms and into the core biology of the disease. By using a sophisticated machine learning model, they have established two clear and distinct patterns of tissue damage in MS patients.
This breakthrough is expected to help clinicians better understand the unique trajectory of each patient's condition, leading to more precise and proactive treatment strategies.
Moving Beyond Symptoms
Traditionally, MS is classified into types like 'relapsing-remitting' or 'progressive'. While useful, these categories describe the clinical course of the disease, not its biological cause. The new research aims to create a classification system based on what is happening to the nerve cells and brain tissue, which could be a more accurate way to guide treatment decisions.
The Science Behind the Discovery
The research team, a collaboration between UCL and Queen Square Analytics, focused on a specific protein in the blood called serum neurofilament light chain (sNfL). Levels of this protein are an indicator of nerve cell damage and can signal how active the disease is.
Data from 600 MS patients, including their sNfL blood levels and detailed MRI brain scans, were fed into a machine learning model named SuStaIn. The AI was tasked with identifying patterns that the human eye might miss.
The algorithm successfully identified two consistent, distinct patterns of disease progression, which the researchers have named based on when sNfL levels rise.
The Two Newly Identified Subtypes
The AI model distinguished between two groups with different biological timelines:
- Early sNfL Subtype: In this group, patients show high levels of the sNfL protein early in their disease course. Their MRI scans revealed visible damage in the corpus callosum, a key part of the brain connecting the two hemispheres. These patients also tended to develop brain lesions more quickly, suggesting a more aggressive and active form of the disease from the outset.
- Late sNfL Subtype: This group follows a different path. Brain shrinkage, particularly in areas like the limbic cortex and deep grey matter, occurs before a significant rise in sNfL levels is detected. This pattern suggests a slower, more insidious disease process where overt damage becomes apparent at a later stage.
Implications for Patient Care
This new understanding of MS subtypes has profound implications for how patients could be treated in the future. By identifying a patient's biological subtype early on, doctors can make more informed decisions about their care.
There are approximately 20 different treatment options available for relapsing forms of MS, but fewer for progressive types. Personalized medicine could help match the right patient to the right treatment more effectively.
Dr. Arman Eshaghi, the study's lead author from UCL, explained the potential impact.
“By using an AI model combined with a highly available blood marker with MRI, we have been able to show two clear biological patterns of MS for the first time. This will help clinicians understand where a person sits on the disease pathway and who may need closer monitoring or earlier, targeted treatment.”
For example, a patient identified with the early sNfL subtype might be considered for higher-efficacy treatments sooner to control the aggressive inflammation. In contrast, someone with the late sNfL subtype might benefit more from therapies aimed at protecting brain cells and neurons from gradual degeneration.
Expert Reaction and Future Outlook
The findings have been met with enthusiasm from the wider medical community. Experts believe this research adds to a growing body of evidence that MS should be defined by its biology, not just its clinical presentation.
Caitlin Astbury, Senior Research Communications Manager at the MS Society, called the study an “exciting development in our understanding of MS.” She noted the limitations of current classifications, stating, “MS is complex, and these categories often don’t accurately reflect what is going on in the body, which can make it difficult to treat effectively.”
The long-term goal is to integrate these AI-powered insights into routine clinical practice. A simple blood test combined with an MRI scan could one day provide a detailed biological profile of a patient's MS, transforming a diagnosis that has remained largely unchanged for centuries.
As research continues, the hope is that this deeper understanding will not only refine existing treatments but also accelerate the search for new therapies that can halt or even reverse the progression of the disease for everyone affected.