Researchers from the University of Surrey have developed an artificial intelligence system that can predict the progression of knee osteoarthritis by analyzing X-ray images. The new technology is designed to forecast how a patient's knee joint will appear one year in the future, potentially transforming how the condition is managed for millions of people worldwide.
The AI model uses machine learning to generate a future image of the knee and assign a disease risk score. This predictive capability aims to help clinicians identify high-risk patients earlier, allowing for more personalized and proactive treatment plans.
Key Takeaways
- Researchers at the University of Surrey created an AI that predicts the one-year progression of knee osteoarthritis using X-rays.
- The system was trained on a massive dataset of nearly 50,000 X-rays from almost 5,000 patients.
- It is reportedly nine times faster and more compact than comparable predictive tools, facilitating easier clinical integration.
- The technology could enable earlier identification of high-risk patients, leading to personalized care and potentially delaying severe joint damage.
- The research team believes this approach could be adapted for other chronic conditions like heart disease and lung damage.
A New Tool for a Widespread Condition
Osteoarthritis is a degenerative joint disease that represents a significant global health challenge. The new AI system, developed at the University of Surrey, offers a novel approach to managing this condition by providing a glimpse into its future progression.
By analyzing a standard knee X-ray, the AI can visualize the expected changes in the joint over the next 12 months. This allows medical professionals to move from a reactive treatment model to a more preventative one. Identifying patients whose condition is likely to worsen rapidly is a critical step in effective management.
Understanding Osteoarthritis
Osteoarthritis is the most common form of arthritis, characterized by the breakdown of cartilage in the joints. This causes pain, stiffness, and reduced mobility. It primarily affects the hands, hips, and knees and becomes more common with age. Currently, diagnosis relies on physical exams and imaging like X-rays, but predicting the speed of joint deterioration in individual patients remains a major challenge.
The system's ability to score disease risk gives clinicians a quantitative measure to guide their decisions. This could help determine the intensity of physical therapy, recommend lifestyle adjustments, or better time interventions like surgery.
The Technology Behind the Prediction
The AI's predictive power is built on a foundation of machine learning. The research team trained the model using one of the world's largest osteoarthritis datasets, which included nearly 50,000 knee X-rays collected from almost 5,000 patients over several years.
This extensive training data allowed the AI to learn the subtle patterns and changes in joint structure that indicate future disease progression. It analyzes features in the X-rays that may not be immediately apparent to the human eye to make its predictions.
"[This tool will] help clinicians identify high-risk patients sooner and personalise their care in ways that were not previously practical," said Professor Gustavo Carneiro, who was involved in the research.
According to the university, the resulting AI model is not only accurate but also highly efficient. It is reportedly nine times faster and more compact than similar predictive technologies. This efficiency is crucial for real-world application, as it means the software can run on standard hospital computers without requiring specialized, high-powered hardware, making it more accessible to a wider range of healthcare facilities.
Addressing a Global Health Burden
The development of this AI is particularly significant given the scale of osteoarthritis's impact. The condition affects a vast number of people and places a considerable strain on healthcare systems globally.
Osteoarthritis by the Numbers
- Over 500 million people worldwide are affected by osteoarthritis.
- It is the leading cause of disability in older adults.
- The condition's prevalence is rising due to aging populations and increasing rates of obesity.
By enabling earlier and more targeted interventions, the technology has the potential to improve patient outcomes significantly. Proactive care could help individuals maintain mobility for longer, reduce chronic pain, and delay or even prevent the need for invasive procedures like total knee replacement surgery.
This shift towards preventative medicine could also lead to substantial cost savings for healthcare systems by reducing the number of surgeries and long-term disability claims associated with severe osteoarthritis.
Broader Implications for Chronic Disease Management
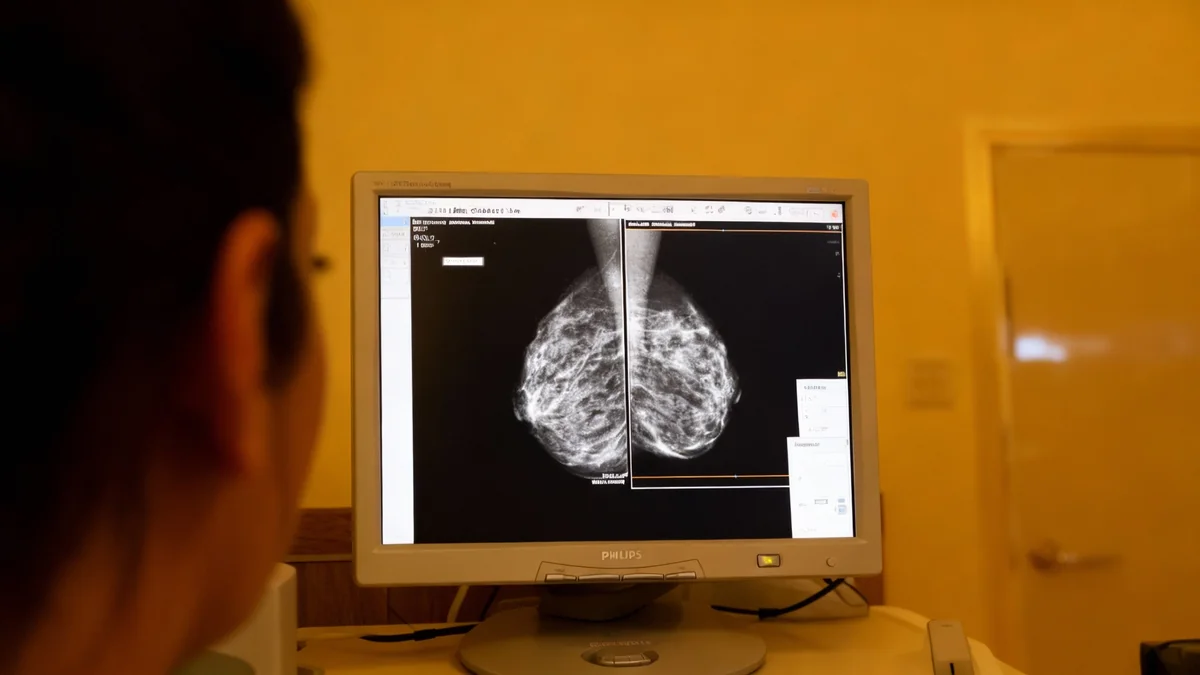
While the initial focus of this AI system is on knee osteoarthritis, the researchers believe the underlying methodology could be applied to a wide range of other chronic health conditions. The ability to predict disease progression from medical images is a powerful concept in modern medicine.
The team suggests the same approach could be adapted for other diagnostic challenges, including:
- Predicting the extent of future lung damage in smokers from chest X-rays.
- Tracking the progression of heart disease by analyzing cardiac imaging.
- Monitoring other forms of degenerative joint disease in areas like the hip or spine.
This potential for broader application highlights a significant shift in medical diagnostics, where AI tools can serve as predictive assistants to clinicians, helping them make more informed decisions long before a condition becomes critical. The core principle is using large datasets to forecast patient-specific outcomes.
Next Steps Toward Clinical Use
The University of Surrey has announced its intention to seek partnerships to help bring this technology from the research lab into real-world clinical settings. The transition will involve further validation studies, regulatory approvals, and integration with existing hospital software systems.
The goal is to create a seamless tool that physicians can use as part of their standard diagnostic workflow. If successfully deployed, this AI could become an invaluable resource for orthopedic specialists, rheumatologists, and general practitioners who manage patients with osteoarthritis.
The development marks another step forward in the integration of artificial intelligence into healthcare, with a focus on creating practical tools that address common and debilitating conditions affecting millions of people.