Researchers have developed a new artificial intelligence model capable of forecasting an individual's potential risk for over 1,000 different diseases throughout their life. The model, named Delphi-2M, represents a significant step in shifting medical practice from diagnosing existing conditions to proactively identifying future health risks.
The details of this large diagnostic model were published in the scientific journal Nature on September 17th. By analyzing complex health data, Delphi-2M aims to provide insights that could enable earlier interventions and personalized preventative care.
Key Takeaways
- A new AI model, Delphi-2M, has been developed to forecast future disease risks.
- The model can predict the likelihood of a person developing one of more than 1,000 medical conditions.
- This technology marks a shift from reactive diagnosis to proactive health management.
- The findings were published in the peer-reviewed journal Nature, highlighting the study's scientific significance.
Understanding the Delphi-2M Model
Delphi-2M is what is known as a large diagnostic model. This type of AI is designed to process and interpret vast amounts of health-related information to identify patterns that are often invisible to human observers. Its primary function is not to diagnose a current illness but to calculate the probability of a future one.
The model's ability to assess risk for over 1,000 distinct conditions is a notable advancement. This wide range covers numerous categories of diseases, from common chronic illnesses to rarer conditions, providing a comprehensive long-term health outlook.
Traditional medical practice heavily relies on a physician's ability to diagnose a disease based on a patient's symptoms, medical history, and test results. Delphi-2M operates on a different principle: it looks for subtle signals and correlations in data to predict which condition a person is most likely to face next, even before symptoms appear.
What Are Large Diagnostic Models?
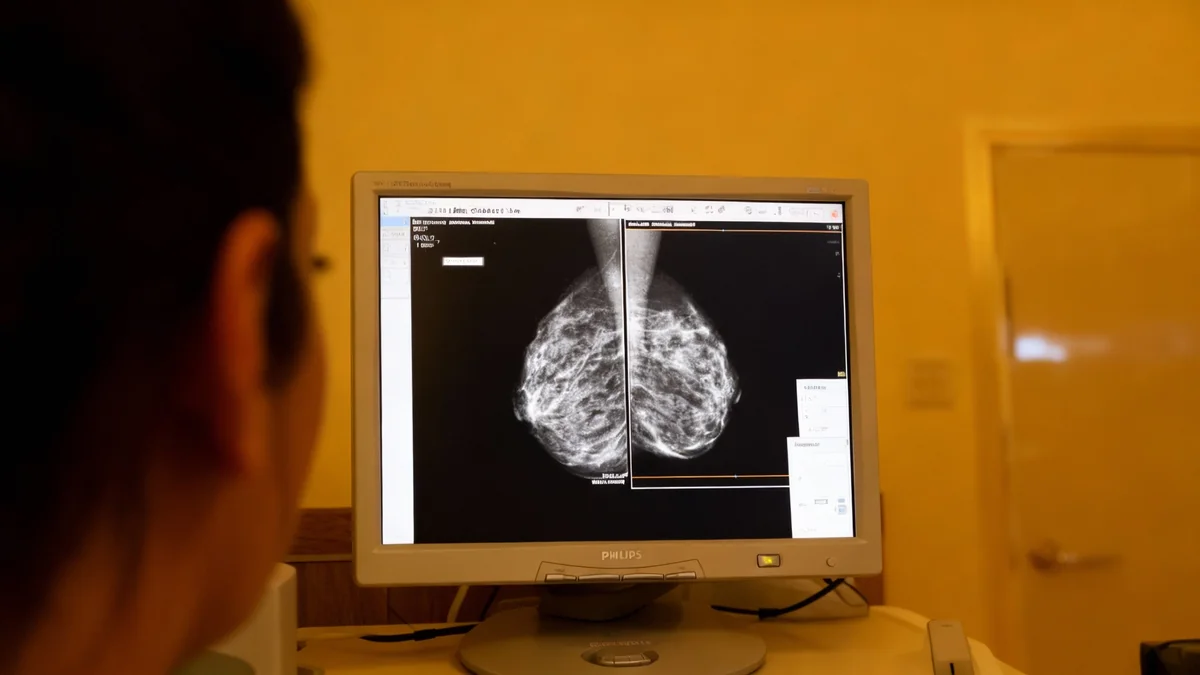
Large diagnostic models are a specialized form of artificial intelligence trained on massive datasets of anonymized electronic health records. These records can include lab results, clinical notes, imaging scans, and genetic information. By learning from millions of patient journeys, these models can identify complex relationships between various health factors and the eventual onset of specific diseases.
The Shift from Diagnosis to Prediction
The development of tools like Delphi-2M signals a potential paradigm shift in modern medicine. For centuries, healthcare has been largely reactive, focused on treating diseases after they have already manifested. The goal of predictive AI is to make healthcare more proactive and preventative.
By identifying individuals at high risk for certain conditions, clinicians can recommend targeted lifestyle changes, earlier screening protocols, or preventative treatments. This approach could significantly improve patient outcomes and potentially reduce the long-term burden on healthcare systems.
For example, if the model flags a patient as having a high risk for developing type 2 diabetes in the next five years, their doctor could implement a personalized plan involving diet, exercise, and regular monitoring to delay or even prevent its onset.
"The art of medicine has long involved working out which disease a patient has. Identifying which diseases a patient might develop in the future is far harder, but no less desirable."
How Predictive AI Models are Trained
The effectiveness of a model like Delphi-2M depends entirely on the quality and quantity of the data it is trained on. These systems are typically fed millions of anonymized patient health records, which serve as a vast library of medical case studies.
Key Data Sources for Training
- Electronic Health Records (EHRs): This includes doctor's notes, diagnoses, prescriptions, and treatment histories.
- Laboratory Results: Blood tests, metabolic panels, and other diagnostic data provide quantitative health markers.
- Genetic Information: Genomic data can reveal predispositions to certain inherited conditions.
- Lifestyle Factors: Information on diet, exercise, smoking status, and environment can also be incorporated.
The AI processes this information to learn the complex, non-linear pathways that can lead to disease. It identifies statistical correlations that might suggest, for instance, that a specific combination of blood markers at age 40 is strongly associated with heart disease at age 60.
The Scale of Data
Large diagnostic models often require datasets containing information from millions of individuals over many years to achieve high levels of accuracy. The diversity of this data is crucial to ensure the model performs well across different populations.
Potential Applications and Future Impact
The practical applications of a reliable disease forecasting model are extensive. If integrated into clinical workflows, Delphi-2M and similar technologies could transform several aspects of healthcare.
Personalized Preventative Medicine
The primary application is in creating highly personalized preventative care plans. Instead of general health advice, patients could receive specific recommendations based on their unique risk profile. This could lead to more effective prevention strategies tailored to the individual.
Optimizing Clinical Resources
Healthcare systems could use this technology to allocate resources more efficiently. For instance, individuals identified as high-risk for certain cancers could be prioritized for earlier and more frequent screenings. This targeted approach ensures that diagnostic tools are used where they are most needed.
Accelerating Medical Research
Researchers could also use these models to better understand disease progression and identify new potential risk factors. By analyzing the patterns the AI discovers, scientists may uncover novel biological pathways or environmental triggers for various illnesses.
Ethical Considerations and Challenges Ahead
Despite its promise, the widespread use of predictive health AI raises important ethical and practical challenges that must be addressed. The accuracy and fairness of these models are paramount.
- Data Privacy: The use of sensitive personal health information requires robust security and privacy protocols to prevent misuse.
- Algorithmic Bias: If the training data is not representative of the entire population, the model may be less accurate for underrepresented demographic groups, potentially worsening health disparities.
- Psychological Impact: Informing a healthy person that they have a high risk of developing a serious disease can cause significant anxiety and stress. Clear communication and patient support are essential.
- Regulatory Oversight: Before these tools can be used in clinical practice, they must undergo rigorous validation and receive approval from regulatory bodies to ensure they are safe and effective.
As research continues, the focus will be on refining the accuracy of these models, ensuring their equitable performance across diverse populations, and developing clear ethical guidelines for their implementation in healthcare settings. The journey from a research paper in Nature to a tool used in everyday medical practice will require careful navigation of these complex issues.