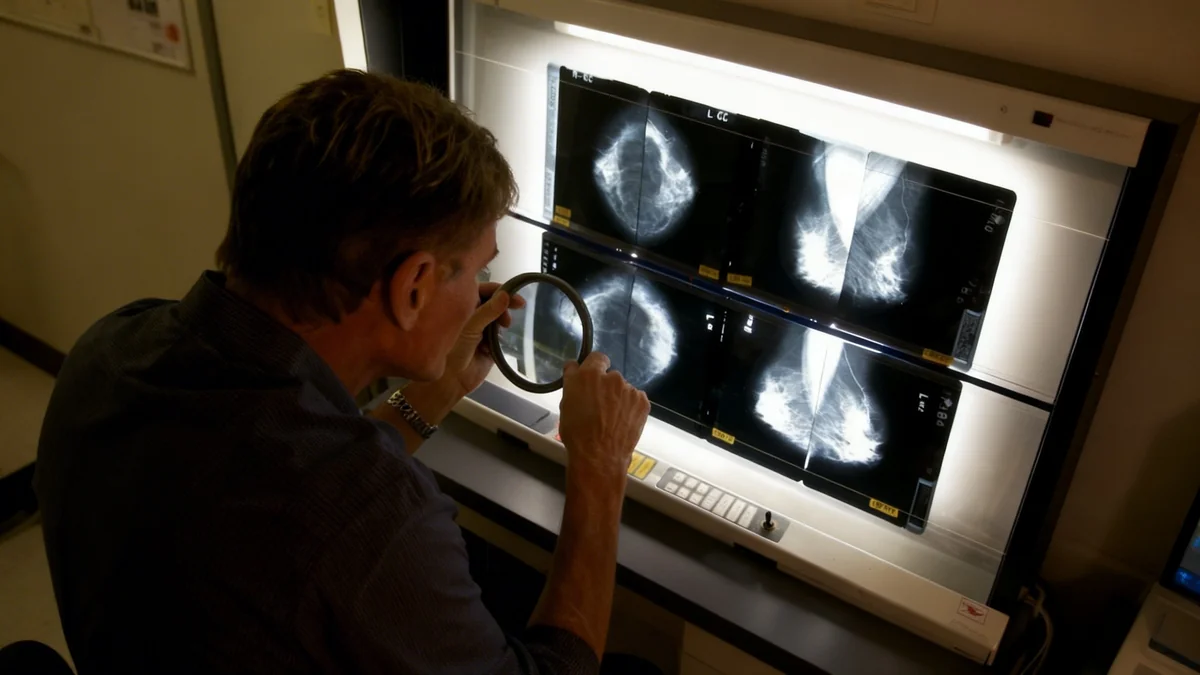
In a surprising turn of events, the field of radiology is experiencing job growth and increased demand, directly challenging long-held predictions that artificial intelligence would make the profession obsolete. Instead of replacing human experts, AI is emerging as a powerful tool that enhances their capabilities, making radiology a key case study in successful human-machine collaboration.
Once cited as a prime candidate for automation, radiology now demonstrates how technology can augment a workforce rather than displace it. New data shows that employment in the field is projected to outpace the national average, driven by AI-powered efficiencies and a growing need for diagnostic imaging.
Key Takeaways
- Artificial intelligence is being used as an assistant in radiology to prioritize scans, improve image quality, and speed up procedures.
- Despite fears of job loss, employment for radiologists is projected to grow 5% by 2034, faster than the 3% average for all occupations.
- Over 1,000 AI-enabled medical devices for radiology have received FDA approval, signaling widespread adoption of the technology as a support tool.
- Experts emphasize that human oversight remains critical, as AI is not a replacement for a radiologist's diagnostic skills and clinical judgment.
A Shift from Fear to Collaboration
Just a few years ago, the outlook for radiologists seemed uncertain. In 2016, Nobel Prize-winning computer scientist Geoffrey Hinton famously suggested that people should "stop training radiologists now," predicting that AI would soon outperform them. This sentiment created a wave of anxiety within the medical community about the future of the profession.
However, the reality on the ground has proven to be far different. Dr. Shadpour Demehri of Johns Hopkins Medicine explained that the technology is now widely viewed as a "second set of eyes." He noted that AI is something that "doesn’t replace anyone, that just makes our job more efficient and more meaningful."
This sentiment is echoed across the industry. The initial apprehension has given way to a collaborative model where technology handles repetitive, data-intensive tasks, freeing up human specialists to focus on complex diagnoses, patient interaction, and treatment planning.
Why Radiology is a Perfect Fit for AI
The field of radiology was uniquely positioned for AI integration. For years, medical imaging like X-rays, CT scans, and MRIs have been digitized. This created vast, structured datasets—the essential fuel for training machine learning algorithms. AI excels at pattern recognition within these large datasets, a core component of a radiologist's work.
Practical Applications in the Clinic
Today, AI tools are actively used in clinics to streamline daily workflows. One of the most significant applications is in triage, where algorithms analyze incoming scans to identify critical cases that require immediate attention. This ensures that patients with urgent conditions, such as a brain hemorrhage or a pulmonary embolism, are prioritized.
Another key area is image enhancement. René Vidal, a professor at the University of Pennsylvania, highlighted AI's ability to create high-quality MRI scans from fewer measurements. This not only improves diagnostic accuracy but also significantly reduces the time a patient needs to spend in the machine.
"That speeds up the process and allows more patients to be seen in the same amount of time," Vidal stated.
Other applications include assisting with the summarization of reports and measuring tumor volumes, though experts note these are still in development. The goal is not to automate the final diagnosis but to automate the preparatory work, allowing radiologists to perform their core duties more effectively.
FDA Approvals Signal Mainstream Adoption
The integration of AI into medical practice is heavily regulated. Any AI tool used for medical purposes must undergo a rigorous review process by the U.S. Food and Drug Administration (FDA). Of the 1,357 AI-enabled medical devices currently approved by the FDA, a staggering 1,041 are for radiology, underscoring the technology's maturity and acceptance in this specific field.
The Data Behind Job Growth
The most compelling evidence against the replacement theory is the employment data. The U.S. Bureau of Labor Statistics projects that employment in radiology will grow by 5 percent from 2024 to 2034. This is notably higher than the average projected growth of 3 percent across all occupations.
Furthermore, job posting data from Indeed confirms this trend, indicating a higher number of available radiology positions in 2025 compared to five years prior. Experts attribute this growth to several factors:
- Increased Demand: An aging population requires more diagnostic imaging, driving up the need for radiology services.
- Enhanced Productivity: AI allows a single radiologist to review more scans with greater accuracy, increasing the overall capacity of a department and justifying the need for more staff to manage the growing workload.
- New Roles: The integration of AI creates new responsibilities related to managing, validating, and overseeing these complex technological systems.
Jack Karsten, a research fellow at Georgetown’s Center for Security and Emerging Technology, observed that AI "is not only not replacing those workers, but it’s actually increasing the amount of work they can do and increasing demand for their services."
Navigating the Risks of a New Technology
Despite the positive outlook, experts caution against unchecked optimism. The adoption of AI in medicine comes with significant risks that must be carefully managed. Dr. Po-Hao Chen of the Cleveland Clinic pointed to the potential for overreliance on automated systems.
One major concern is algorithmic bias. A 2022 study from MIT revealed that an AI model could accurately predict a patient's race from a medical image like an X-ray, even though this information is not visible to human radiologists. This raises serious questions about whether AI could perpetuate or even amplify existing biases in medical diagnoses.
Dr. Chen also expressed concern about the temptation for healthcare administrators to make staffing changes based on AI's capabilities, such as replacing a specialist with a less-qualified practitioner assisted by an algorithm. He warned that while this might work for simple cases, it could be dangerous for detecting complex conditions like cancer or severe infections.
"We have to understand that a lot of the performance of the algorithm comes from the fact that the automation output is reviewed by an expert," he said. "And together, this collaboration, if you will, between the machine and the expert is what makes the improvement real."
The consensus is clear: AI is a tool, not a replacement. Its success depends entirely on the expertise of the human professionals who wield it, ensuring that the final medical decisions are made with the nuance, context, and empathy that only a human doctor can provide.